Several factors are speculated to increase risk of ACL injury in females including lower extremity alignment (wider pelvis, knee valgus, foot pronation), joint laxity, hamstring flexibility, muscle development, hormonal differences, and ACL size (4,6). These are the facts stated in the research, but that is not what I want to discuss here in this post.
What needs to come to the forefront is a phenomenon in sports that we refer to as benign neglect. We see this in a number of sports and it is essentially the acceptance of certain injuries as "just a part of the process", as opposed to trying to change the situation for the better. I have given talks in the past about this benign neglect in the sport of hockey when it comes to groin pulls and sports hernias. For years it has been forged into the culture of hockey that groin pulls will happen, and so much so that they are commonly referred to as "training camp injuries", but this topic is for a future post. Creating change oftentimes takes people who are outside the culture of the sport to stand up and call out a situation of benign neglect.
Today I will discuss this topic in the sport of high school girls basketball, and I'm sure you have already figured out that the injury topic will be ACL tears. This discussion was sparked by a meeting I had last week with a local girls basketball player who tore her ACL this past season and her mother. This was a very open and honest conversation and we discussed her recovery process, but there needed to be more this time. I said "this time" because Andrea has been here before. Last year at this time Andrea had just finished up her post-rehab program with me at Lewis Fitness & Performance. During the spring of 2014 she tore her left ACL during the AAU basketball season, she began her recovery program with us in August of 2014.
By April she was cleared to play basketball and began another grueling AAU schedule full of tournaments and travel. Her schedule did not allow for her to continue in a strength & conditioning program of any kind, and when her basketball team began their pre-season work here at LFP she was tied up in her golf season. She managed to get 3 or 4 sessions with the team, despite having a great golf season where her team won the state championship. She displayed that her strength was still being maintained and things were looking great heading into the fall. But as a strength & conditioning coach you always worry about the athletes you have guided through their recovery when they haven't been able to work consistently with our program. And what you worry about most is the knee on the opposite side of the surgery, as that knee is statistically more at risk then the surgically repaired one.
As the season begins more bad news as one of the freshmen, Addy, tears her ACL in the first game of the season.
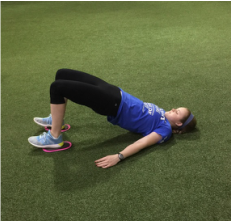
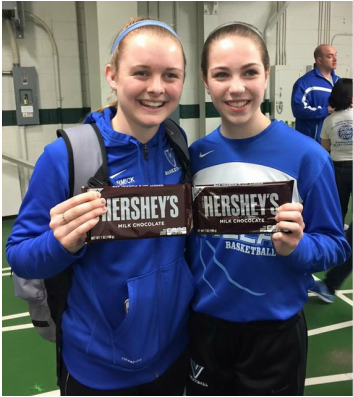
So Addy and Andrea have started down the road to recovery. These are two of the hardest working young ladies that we have worked with here at LFP so I have no doubt that they will do fantastic. Here are some of the activities that these two have started back doing in there first week.
I was completely open and transparent with them. I told them how I felt when Addy hurt her knee, and how I was heading down the road of "benign neglect" thinking that you should probably expect 1 ACL per year, and a freshman who is being exposed to a top notch high school girls basketball program for the first time would be more prone to it. Plus her injury was not a complete non-contact related tear. Then when Andrea went down my heart sank. She had worked so hard.
The first thoughts were that of self reflection. I put our program in front of the mirror and dissected it, ripped it apart for answers as to why this would happen to a young lady that did so well in our program. Had the program changed since she went through it...YES. I will never be able to look back through 7 months of programming and say we haven't changed anything in our program because it is always evolving and improving. But there was nothing to question that was not right on point with those leading the industry in both rehabilitation and sports performance training. The program was not/is not the issue... consistency was.
This is the most important point of this post, and is the missing step in all return to play protocols. When you get CLEARED from your doctor it is now time to fully immerse yourself in a sound strength & conditioning program with no restriction. As a strength & conditioning professional we can now set a progression that will teach an athlete to control their body in a controlled environment to relearn to change direction and then progress to and open, reactionary environment, that is as close to the basketball
court as we can get as far as mimicking the sport environment. At this point we can give the athlete complete confidence that they are fully rehabilitated. At LFP we will have completed a thorough movement evaluation, including the Functional Movemet Screen, to determine movement competency and compensation patterns to aide in the development of their program. But this program must continue, even in-season, as any backtracking in strength/stability/mobility or compensation away from the previously injured ACL will put the other leg statistically in jeopardy.
Consistency is the linchpin in this equation. Getting back to the conversation with Andrea, I told her she can never stop her training. She has 4 Division I offers and 2 ACL surgeries under her belt. I was up front with her and told her the truth... If she tears another the potential to increase her offers will be gone and the 4 offers would likely decrease. I gave her my honest opinion but she already knew. I also told her she must be consistent and I would do whatever was needed to continue her development. This will lead to decreased sleep for us at LFP because I am almost certain we will see her at 5:00am this fall during golf season, because she is a fighter and she knows now that the fight can never stop.
I titled this post the way I did to get your attention, but I also titled it because I never want to enter one of MY daughter's sporting events and have that question cross my mind. And I also don't want anyone to have to console their daughter/son the way that Scott is for Addy in the picture above. I know that won't happen, injuries will always be a part of sports. But I also know we can decrease the likelihood of that happening through scientifically based programming, sound coaching technique, and consistency.
- American Academy of Orthopaedic Surgeons, July 2007, Anterior Cruciate Ligament Injury: Surgical Considerations, http://orthoinfo.aaos.org/topic.cfm?topic=A00297#A00297_R4_anchor (July 11, 2008).
- Griffin LY. Noncontact Anterior Cruciate Ligament Injuries: Risk Factors and Prevention Strategies. Journal of the American Academy of Orthopaedic Surgeons. 2000;8:141-150.
- Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. American Journal of Sports Medicine. 2006 Feb; 34(2):299-311.




 RSS Feed
RSS Feed